HIT Consultant – Read More
What You Should Know:
– A new brief utilizing the latest 2024 Health Information National Trends Survey (HINTS) data reveals significant progress in patient and caregiver access to online medical records and patient portals. The report also highlights that nearly all non-federal acute care hospitals in the U.S. were engaged in electronic public health reporting in 2024, a crucial step in modernizing public health data exchange. However, despite marked progress, more than 8 in 10 hospitals experienced at least one challenge to electronic public health reporting during the year.
– Improving seamless, secure public health data exchange between healthcare and public health agencies (PHAs) remains a key goal of data modernization efforts. The Centers for Disease Control & Prevention (CDC) launched its Public Health Data Strategy (PHDS) in 2023 to address gaps, remove barriers, and improve data availability for public health decision-making and population health.
High Rates of Electronic Public Health Reporting
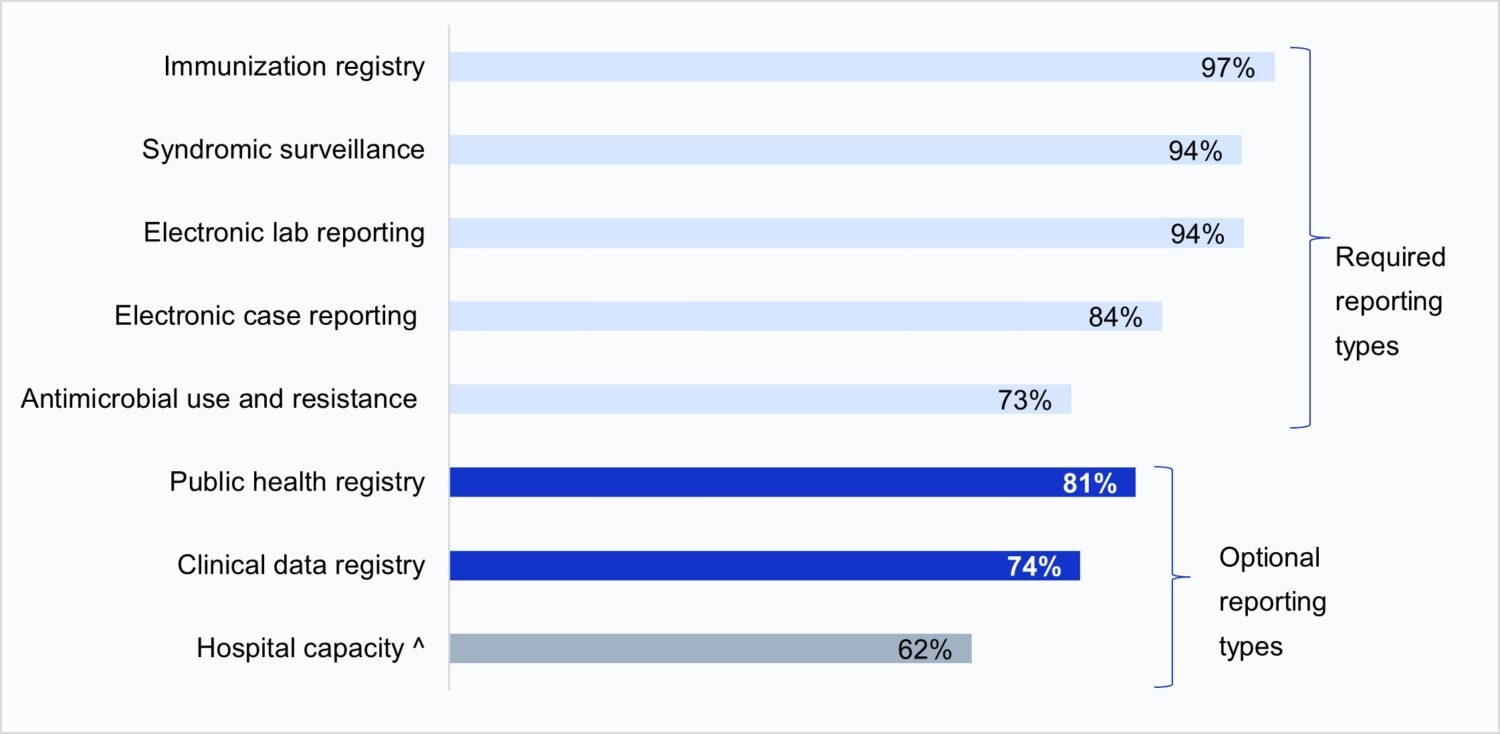
In 2024, nearly all hospitals were engaged in electronic public health reporting for core (required) data types: immunization, syndromic surveillance, laboratory, and case reporting. Rates were highest for these core data types, which have been required by the Centers for Medicare & Medicaid Services (CMS) Medicare Promoting Interoperability (PI) Program since 2022.
Key findings on reporting engagement include:
- Nearly three-quarters of hospitals were electronically reporting Antimicrobial Use and Resistance (AUR) data shortly after it became required in January 2024.
- Rates of electronic public health reporting have increased over time for both required and optional reporting types (e.g., public health and clinical data registry reporting).
- Electronic case reporting saw a substantial increase from 53% in 2021 to 84% in 2024, following its requirement in the PI program in 2022.
- Hospital engagement in public health and clinical data registry reporting (which qualify for bonus points but are not required) also increased significantly between 2021 and 2024 (from 65% to 81% and 50% to 74%, respectively).
EHRs Dominate Submission Methods, Automation on the Rise
Electronic Health Records (EHRs) were the most common method used to submit data for electronic public health reporting in 2024. Most hospitals submitted data directly through their EHR for core data types, ranging from 71% for electronic case reporting to 86% for immunization registry reporting. Health Information Exchange (HIE) organizations were also commonly used, especially for core data types, though their use varied by state.
While about half of hospitals submitted data directly from their EHR for public health registry, clinical data registry, and AUR reporting, portals and flat files were still commonly used for these optional reporting types.
Automation is also becoming prevalent:
- Fully or primarily automated processes were predominantly used for core data types, including immunization (84%), syndromic (82%), lab (78%), and case (61%) reporting.
- However, newly required and optional reporting for AUR, public health registry, clinical data registry, and hospital capacity reporting primarily occurred through a mix of automated and manual processes. About one-third of hospitals still use fully or primarily manual processes for hospital capacity reporting. Automated reporting is mutually beneficial, reducing provider burden while improving data timeliness and accuracy for PHAs.
Variances in Reporting Engagement by Hospital Characteristics
Hospital engagement in electronic public health reporting varied by hospital characteristics. On average, hospitals were engaged in about 6 out of 8 measured reporting types, and nearly all core types (3.5 out of 4).
However:
- Small, rural, independent, and critical access hospitals were engaged in fewer types of electronic public health reporting on average compared to their larger, urban, system-affiliated counterparts.
- Hospitals using the market-leading EHR vendor engaged in more types of electronic public health reporting compared to hospitals utilizing non-market-leading vendors (6.7 vs. 5.8 on average).
- Small, rural, independent, and critical access hospitals, as well as those not using the leading EHR vendor, had significantly lower rates of submitting data directly through the EHR for core reporting types.
Persistent Challenges to Public Health Reporting
Despite significant improvements, hospitals continue to face substantial challenges. In 2024, 81% of hospitals reported at least one challenge to electronic public health reporting, with an average of about 3 out of 7 challenges reported.
The most common challenges reported overall were:
- Technical complexity of interfaces, transmission, or submission processes (55%).
- Perception that PHAs lack the capacity to electronically receive information (50%).
Challenges were highest for electronic case reporting (59%) and AUR reporting (57%), potentially due to these types recently becoming required by the CMS PI program. About a third of hospitals also reported onboarding and cost-related challenges, while a quarter found it difficult to extract relevant information from the EHR. Notably, only 19% of hospitals reported no major challenges for any reporting type.
The Path Forward: Standards, Collaboration, and Modernization
The COVID-19 pandemic exposed enduring gaps in the public health data infrastructure that still hinder the use of electronic, standardized data sharing. Ongoing federal efforts aim to address these issues, including the CDC’s PHDS focus on automated solutions, and ASTP/ONC’s Health IT Certification Program requiring developers to enable standardized data submission to PHAs. The United States Core Data for Interoperability (USCDI+) Public Health Initiative is also working towards a standardized set of data elements to support public health use cases.





