HealthPopuli.com – Read More
As I track the phenomenon of health citizenship in the U.S., I observe growing consensus among American patients increasingly impatient for health care access. We can now add Americans’ growing dissatisfaction with the prior authorization process, an opinion that now spans majorities of consumers regardless of their political party ID. As the title of the latest Kaiser Family Foundation health tracking poll summarizes it in their analysis, the Public Finds (the) Prior Authorization Process Difficult to Manage.
![]()
The first chart from the KFF poll tells us that 3 in 4 (73%) U.S. adults believe that denials and delays of health care services by health insurance companies are a major problem. Another 21% of people say these denials are a “minor” problem, netting to 94% of Americans saying prior auth is problematic.
That includes 57% of Republicans calling out denials of care as a “major” problem and a substantial 34% saying such denials are a minor problem. ![]()
Another lens on this issue looks at Americans by household income and primary insurance coverage, which you might surmise could yield significant differences across these fiscal demographics.
However, the disparities among consumers’ of lower incomes (say, below $90K for households) compared with families earning $90K aren’t so dramatic.
Compared health plan type and its influence on consumers’ views on delays and denials from prior authorization, we also see relatively small differences — with fewer of those Medicare members citing a major problem (67%) compared with three-quarters of enrollees in employer-sponsored plans or self-purchases plans. Slightly more people insured via Medicaid cite “major” problems than members of these other plan types.
![]()
Experience is our teacher when it comes to health care denials: one-half of insured Americans have been required to get prior authorization before receiving a treatment in the past two years, the next chart illustrates. Here, we see slightly higher P.A. requirements for people enrolled in Medicare (55%) and Medicaid (53%) versus commercial insurance.
![]()
Health Populi’s Hot Points: Here’s where the health care access challenges’ rubber hits road among those U.S. insured adults whose health insurance companies delayed or denied care of treatment, service, or medication requested by their doctor.
Overall, 29% of these consumers’ had delayed or denied care, split by insurance plan type as follows:
- 33% Medicaid
- 31% employer-sponsored insurance
- 29% self-purchased plan, and,
- 25% Medicare.
In late June, health insurance companies’ leadership convened with the Centers for Medicare and Medicaid Services, including Secretary of HHS Robert F. Kennedy, Jr., and CMS Administrator Dr. Mehmet Oz, to agree on a set of principles to address prior authorization problems. The improvements would address transparency, standardization, improving communication and real-time responsiveness, and other aspects of improving the P.A. process for patients and families.
KFF found that as of mid-July, a couple of weeks since this voluntary agreement was struck, only 1 in 5 Americans had heard of the Health Insurance Initiative to reduce the burden of prior authorizations. Furthermore, few consumers (about one-third_ thought it likely that the health insurance companies would follow through on the promises to improve prior authorizations.
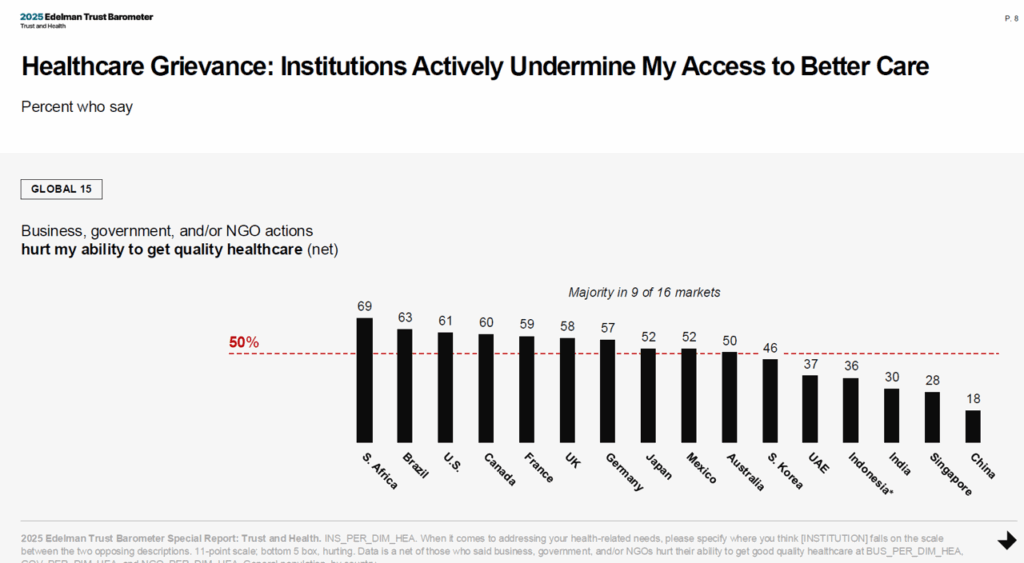
For health care in the U.S., and in particular, the health insurance industry, we are living and operating in an Era of Grievance — a key finding from the 2025 Edelman Trust Barometer which has serious implications for patients and providers trying to receive and deliver care every day. While this is not a sole American challenge as the last chart informs us, health citizens in the U.S. nonetheless bear heavier senses of grievance when it comes to peoples’ ability to get quality care in America.
The post Prior Authorizations Are a Problem for People in the U.S., Regardless of One’s Political Party, Income, or Insurance Type appeared first on HealthPopuli.com.





