HealthPopuli.com – Read More
The costs of medical care are breaking the system, PwC asserts at the start of its new report on the $1 trillion opportunity to reinvent healthcare. The past 3 years of 8+% U.S. national health expenditure increases are “untenable,” PwC says, with 90% of that spending going toward patients with chronic and mental health conditions. 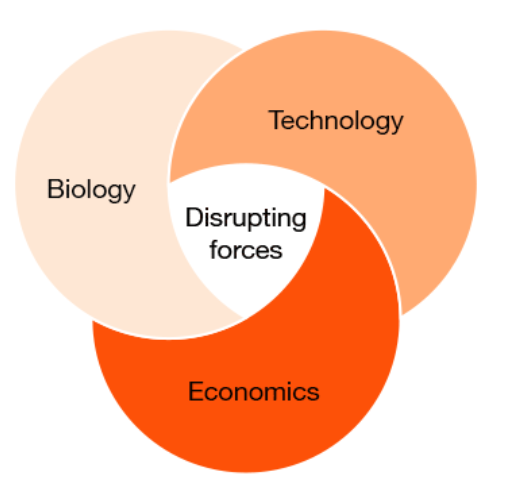
What will transform the system and move us from “breaking point to breakthrough?” Biology and technology, PwC explains, with technology moving exponentially and simplifying care at scale, and biology decoding the “human operating system” enabling precision at scale.
This $trillion opportunity will require a lot of disruption between now and 2035, exposing “cost pools” — that is waste, duplication, opportunity to streamline — in the process challenging the business models and incentive structures of legacy health care stakeholders: hospitals, health plans, pharma, and med-tech companies.
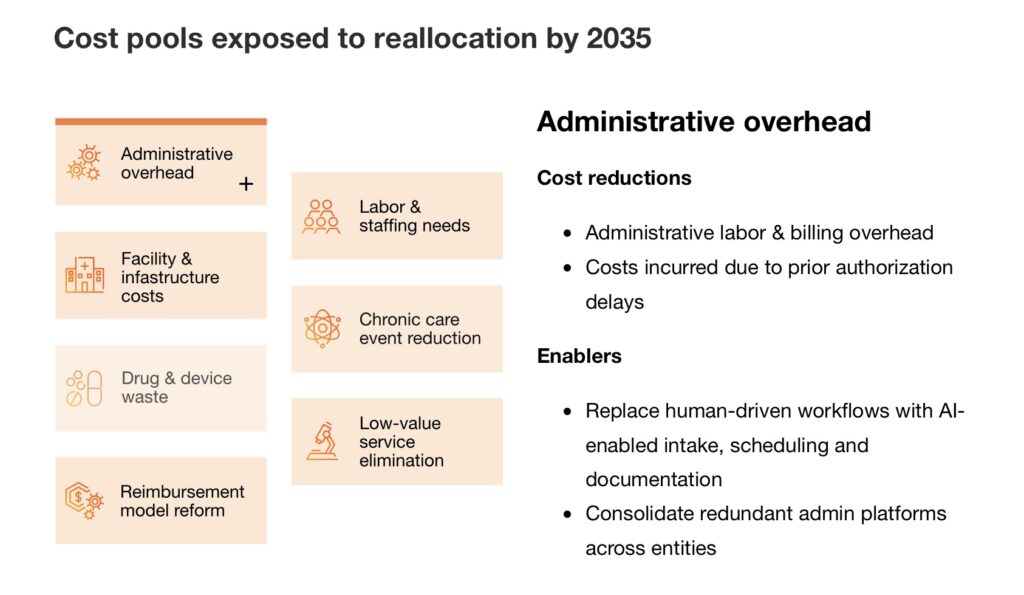
PwC details the cost groupings or pools that would be reallocated by 2035, addressing,
- Administrative overhead
- Facility and infrastructure
- Drug and device waste
- Reimbursement reforms
- Labor and staffing
- Chronic care reduction, and,
- Low-value service elimination.
Keep in mind those “cost pools” can represent operating/profit margins of the stakeholders — so disruption, which is used all too often in business strategy-speak, in this case is the proper word to use.
The new operating model for health care 2035 would put consumers-first with enchantingly- and co-designed services in bundles and seamless delivery. These will be virtual-first when optimally channeled that way, before the physical brick-and-mortar face-to-face tradition, enabled through AI-powered data-enriched engines and algorithms. And, partnerships — some disruptive, to be sure — will populate the health/care ecosystem, enabling franchise-type models that also ensure governance for shared and fair/equitable data treatment.
In this vision, public health is personal health, the home is the medical home, and hospital-to-home is just a part of omni-channel, platformed health care delivery — site neutral, but transformational along the way.

Health Populi’s Hot Points: In constructing scenarios on the future of health care in 2030, I created four alternative futures shown here as part of my AHIP 2024 collaboration with the health plan conference.
Over the past couple of years, and certainly in 2025 and now reviewing 2026 short-term forecasts for U.S. health care, we are witnessing a pull to the “south” of the Y-axis, away from collective/public health toward a more individually-driven health policy ethos.
As we move “south,” we face two futures both of which we can hold in our minds at the same time — a feeling of being Castaway as an individual, confronting a fragmented and bureaucratic medical care labyrinth; as well as evolving into being CEO of healthcare for ourselves and our loved ones with more private pay, out-of-pocket, and so-called consumer-driven health care options (think: Hims & Hers, Ro, and other direct-to-patient [DTP] options, among a growing proliferation of self-care models that compete for dollars in the household budget). 
PwC’s research found that roughly one-half of U.S. adults would be willing:
- To adopt AI-powered treatment such as analytics to tailor care plans and treatment and provide health updates and triage
- To use robots in lieu of people for drone delivery of test kits and medications, along with smart home health sensors to monitor vitals
- To consume drugs tailored to one’s DNA for genomic screening to assess risk and guide care, along with personalize meds and treatments based on genetics, and,
- To unify health records across provides ands hare medical data to accelerate clinical trials.
Those incumbents across the four stakeholder areas that are “believers” in PwC’s characterization of leadership for 2035 health care will bravely face the cost-pool challenges while re-imagining care and the role the organization’s business plays in the many collaborations that will be successful in the coming decade. PwC reminds all of us that, “the critical test for the future of health will be whether a major industry outsider — free from legacy infrastructure but armed with capital — will have the vision, insight and resolve to disrupt healthcare.”
Thanks to the PwC team for giving us this rich food-for-thought especially in our season of planning for 2026 and beyond…
The post In 10 Years, Health Care Will Happen Where Life Happens – PwC’s Tea Leaves into 2035 appeared first on HealthPopuli.com.