MedTech Intelligence – Read More
Medical device innovation is accelerating across nearly every therapeutic area. Software-enabled platforms, connected devices, and artificial intelligence are reshaping how products are conceived, developed, and deployed in clinical practice. Yet for many large, established medical device companies, development timelines, cost predictability, and execution efficiency have not improved at the same pace.
The constraint is rarely a lack of ideas, investment, or technical talent. Instead, it is R&D operations—the interconnected system of processes, digital platforms, governance models, and decision-making mechanisms that convert innovation into approved, manufacturable products. In many mature organizations, these operating models were designed for a different era and now struggle to support the scale, speed, and complexity of modern device development.
The Scale and Complexity of Today’s MedTech Environment
The broader industry context makes these operational challenges more visible. According to the 2024 AdvaMed Annual Report, the global medical device industry now represents nearly $600 billion in economic output, supported by sustained R&D investment and continued expansion into new clinical applications.
Regulatory activity reflects this scale. Across its medical device programs, the U.S. Food and Drug Administration (FDA) processes thousands of submissions each year, including large volumes of 510(k) clearances and a steady flow of premarket approval (PMA) applications for higher-risk technologies.
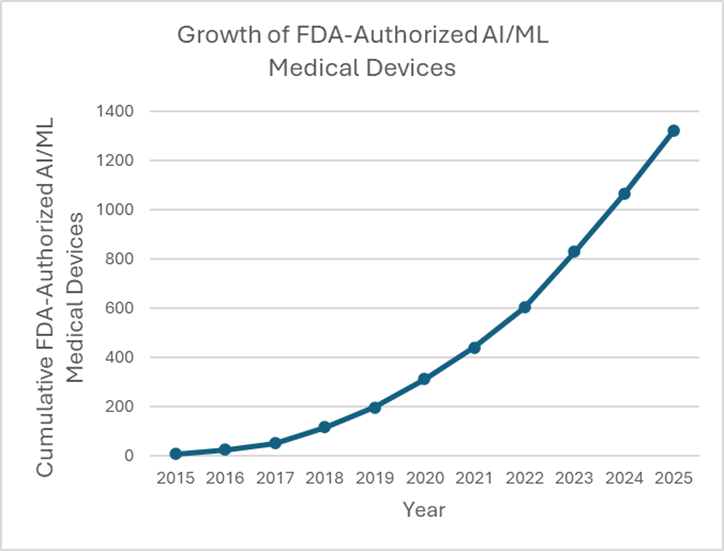
At the same time, product complexity is rising rapidly. As of mid-Dec, 2025, the FDA has now authorized nearly 1,350 Artificial Intelligence and machine learning (AI/ML)–enabled medical devices, compared with only a few dozen a decade ago.
These products introduce new development challenges: continuous data learning, algorithm validation, cybersecurity considerations, and expanded post market monitoring requirements. Collectively, they place far greater demands on how R&D data is generated, connected, reviewed, and maintained.
How Legacy R&D Operations Took Hold
In large MedTech organizations, fragmented R&D operations are rarely the result of poor leadership or lack of discipline. More often, they are the cumulative outcome of long-term success.
Over decades, companies adapted their processes to meet evolving regulatory expectations, expanded portfolios across multiple therapeutic areas, entered new geographic markets, and integrated acquisitions. Each step solved a real business problem at the time. However, the result in many organizations is a patchwork of partially connected systems—multiple product lifecycle management (PLM) tools, quality management systems (QMS), document repositories, and homegrown workflows that do not fully interoperate.
What once provided flexibility now introduces friction. Engineering data, risk analyses, verification evidence, and regulatory documentation often live in separate systems, requiring manual reconciliation at critical-decision points.
Where R&D Operations Loses Time
Operational inefficiencies rarely appear as single, visible failures. Instead, they accumulate quietly. Teams spend weeks aligning requirements across systems, reformatting information for design reviews, or repeating tests because upstream assumptions were not fully resolved. Design reviews become status updates rather than decision forums. Risks that could have been mitigated early are pushed downstream, where changes are more expensive and more visible to regulators.
In many organizations, development processes evolved primarily to demonstrate audit readiness rather than decision readiness. Documentation exists, but it does not always support timely, high-confidence decisions. The result is longer development cycles without corresponding gains in quality or predictability.
Why Modernization Is Especially Difficult in MedTech
Modernizing R&D operations in a regulated industry presents constraints that are not easily addressed with standard digital transformation playbooks.
Core systems often require validation, making large-scale replacements slow and risky. Business continuity concerns limit tolerance for disruption, particularly for sustaining engineering activities tied to marketed products. Global regulatory variation demands consistency without rigidity, further complicating system design.
Cultural factors also play a role. Processes that have passed prior inspections are often treated as untouchable, even when they no longer scale effectively. As a result, modernization initiatives frequently stall or deliver incremental benefits that fall short of expectations.
What Industry Benchmarking Reveals
Industry benchmarking consistently points to integration—not additional tools—as a key differentiator. Deloitte’s MedTech R&D and product development benchmarking highlights that organizations with stronger alignment across R&D, quality, and regulatory functions experience fewer late-stage surprises and more predictable submission outcomes. Notably, these organizations do not necessarily have fewer processes or lighter governance. Instead, they design operations to support end-to-end decision flow, ensuring that data generated in one phase of development directly informs downstream activities.
What Actually Works in Practice
Organizations that successfully improve R&D performance tend to focus on a small set of pragmatic principles.
First, they design operating models around decisions, not documents. Critical technical, clinical, and regulatory decisions are explicitly defined, with clear criteria and accountable owners.
Second, they invest in evidence connectivity—linking requirements, risk management, verification, and clinical evidence into a coherent, traceable system. This improves both internal efficiency and regulatory confidence.
Third, modernization is executed in layers. Rather than replacing validated core systems, organizations enhance integration, analytics, and workflow orchestration around them, reducing risk while restoring connectivity.
Finally, governance mechanisms such as design reviews and phase gates are used to resolve issues, not defer them. Clear decision expectations reduce rework and compress timelines without compromising rigor.
Key Takeaway for MedTech Leaders
Large medical device companies are rarely constrained by a lack of innovation, talent, or investment. They are constrained by aging, fragmented R&D operating models that no longer match the complexity of today’s products.
Sustainable improvement does not come from cutting processes or bypassing controls. It comes from restoring connectivity between decisions, data, and accountability across the R&D lifecycle—allowing teams to move faster while maintaining regulatory confidence and product quality.
The post R&D Operations Bottlenecks in Large Life Sciences Organizations: What can MedTech Leaders Do? appeared first on MedTech Intelligence.