HIT Consultant – Read More

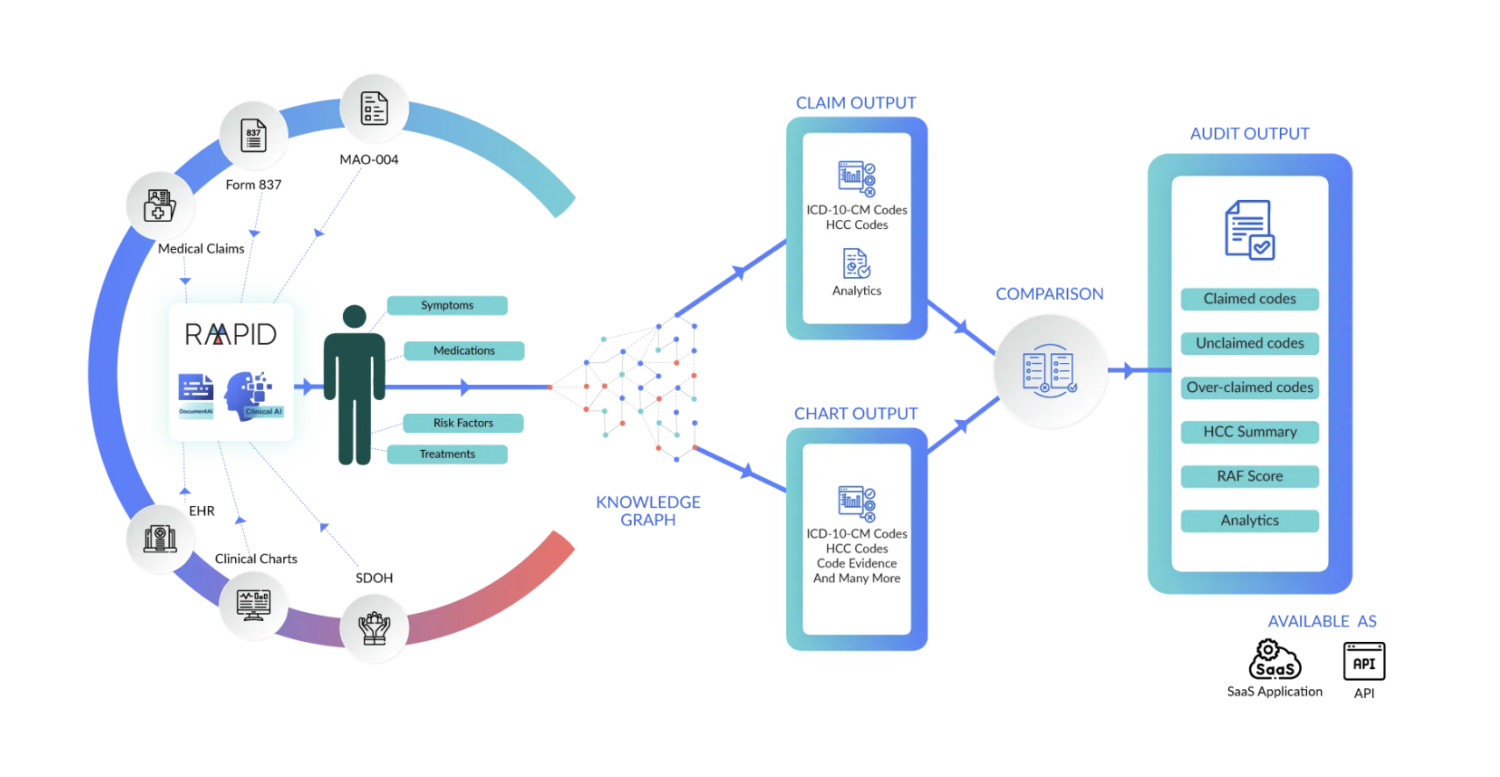
As healthcare organizations deepen their investments in value-based care, one obstacle continues to stymie progress: incomplete visibility into the patient’s health status. The problem isn’t limited to a single source, such as claims data, though claims are often blamed. Rather, it’s the fragmented nature of healthcare data itself. Patient information is dispersed across a patchwork of systems—EHRs, HIEs, scanned documents, specialist consults, diagnostic reports, lab results, payer files, and hospital notes—and it exists in multiple formats: structured fields, free-text notes, image annotations, and audio transcripts.
Each source captures part of the story. But none offers a complete picture on its own. Clinicians are left to piece together patient narratives from these disparate fragments, often under tight time constraints and with little confidence in the completeness of what they’re seeing. Making sense of the flood of multi-source, multi-modal data is an inhuman challenge.
This chronic failure to rise to this challenge goes beyond mere inconvenience to directly affect clinical and financial outcomes. Inaccurate or incomplete documentation can lead to under-coding, poor risk adjustment, and ultimately lost revenue or regulatory risk. Worse, it can delay diagnoses or result in suboptimal treatment decisions. But when clinicians are given recommendations based on a broad range of sources, their confidence rises accordingly. Based on our own research, we’ve found that diagnosis suggestions based solely on claims data are accepted by physicians less than half the time. When the same suggestions are supported by reconciled multi-source clinical evidence, acceptance rates jump to nearly 80%.
The path forward lies in bringing together data from across systems and modalities into a single longitudinal patient record. AI has made it possible to mine unstructured notes and scanned documents for clinical meaning, align them with structured data, and surface suggestions backed by transparent, verifiable evidence. But even the best data pipelines still rely on a critical input that’s often missing: the visit itself.
The clinical encounter remains the most direct, real-time window into the patient’s current state. But all too often it is treated only as an output for documentation. This is where ambient visit transcription fundamentally changes the game. By “simply” listening to the conversation between patient and clinician, ambient technology transforms the encounter into a new source of structured, actionable data.
Ambient transcription conjures an image of an automatic stenographer, but this technology goes beyond recording: it actually understands the visit. It distinguishes between speakers, identifies clinical concepts, and captures clinical nuance. A patient sharing sleep disturbances or mood changes, for instance, might point to underlying depression. When paired with historical data, such as a documented history of diabetes or hyperlipidemia, these insights can prompt a more complete diagnosis. Rather than relying solely on previously coded conditions, clinicians gain real-time visibility into what’s changed, what’s resolved, and what new issues are emerging.
This kind of dynamic reconciliation, which bridges historical records with the live clinical moment, has enormous implications for risk adjustment. Visit notes are not only up to date, but can be reviewed almost instantly, integrated into the longitudinal patient record, and immediately considered in care decisions and coding workflows. This eliminates the documentation lag and ensures that new conditions aren’t overlooked due to system delays or transcription errors.
Moreover, ambient-derived notes improve clinician trust. Unlike suggestions generated from decontextualized claims files, ambient data is rooted in the clinician’s own conversation and is more immediate and relevant by its very nature. When these notes are layered on top of multi-source reconciled data, the result is a far more complete picture of the patient’s health.
The clinical and operational impact is clear. Documentation burden drops. Acceptance of coding suggestions rises. Missed diagnoses decline. And most importantly, clinicians can spend more of their cognitive energy on care, rather than chasing data.
Value-based care will never succeed if it relies on overburdened clinicians navigating fragmented systems. The key lies in empowering those clinicians with data that’s reconciled across sources and modalities, interpreted in the context of the live visit, and returned to them not as noise, but as clarity: a coherent, confident insight.
When we treat every encounter as an opportunity to enrich the patient record and provide more comprehensive care, we move closer to the real promise of value-based care: proactive, personalized, and precisely documented medicine.
About Shay Perera
Shay Perera is the co-founder and Chief Technology Officer of Navina, a pioneering AI company transforming how clinicians access and use health data. At Navina, Shay applies his expertise in AI and big data to address a critical challenge in healthcare—preventing vital medical information from being overlooked. Inspired by a personal story of delayed diagnosis in his own family, he co-founded the company to ensure that clinicians have access to actionable, evidence-based insights at the point of care. Shay leads a diverse team of developers, AI researchers, clinicians, and product professionals, driving the creation of an AI-powered platform now used by thousands of clinicians to improve care for millions of patients.