MedTech Intelligence – Read More

Insights shared by industry relative to healthcare and the advancement of medical technology.

Rajani Kumar Sindavalam is a Senior Technical Manager/Medical Device Leader at HCL America Inc.
Frequently, the responsibility for ensuring the safety of a medical device falls on the manufacturer. While this is partially accurate, each manufacturer is obligated to design their devices in a manner that is both safe and effective. However, it can be quite difficult, if not impossible, for a manufacturer to consider the perspectives of all potential medical devices from other manufacturers that may be utilized in conjunction with their own devices in the healthcare setting.
For instance, if your medical device requires several connections to function as intended, ensuring safety can be achieved by designing each connection or socket uniquely to prevent any potential misconnections. As a manufacturer, it is possible to implement procedures within the organization to guarantee that all devices produced adhere to a standardized methodology. However, it is impractical for a designer to consider every product available in the market and to design their product to mitigate all potential misconnections.
As patient acuity rises and the population ages, hospitals increasingly depend on medical devices that are vital for diagnosis, treatment, and rehabilitation. Given that Emergency Rooms and Operating Rooms utilize numerous medical devices simultaneously, there is a significant risk of hospital staff inadvertently making misconnections, despite exercising considerable caution.
Numerous complaints have been reported concerning misconnections that have led to serious injuries or fatalities. Below are several instances from the FDA database. (1).
Example 1: Epidural tubing was erroneously connected to the IV tubing for a patient which resulted in patient death.
Example 2: IV tubing erroneously connected to trach cuff for a child in pediatric care unit resulted in the death of child.
Example 3: IV tubing erroneously connected to the nebulizer for a patient. The misconnection was identified in time by the respiratory therapist to intervene and save the life of the patient.
These instances illustrate how easily a misconnection can occur. The primary reason for this is that many connectors are designed in a similar manner. Consequently, they do not prevent misconnection when hospital personnel attempt to make a connection.
Hospitals employ various manual controls to avert such misconnections. These controls include:
- Conducting manual tracing of each line from the source to the destination
- Labeling the lines at both the source and destination points
- Utilizing color markers to distinguish between different lines
- Implementing line organizers.
These controls are labor-intensive and do not ensure the absence of misconnection. In a rapidly moving hospital setting, such manual processes hinder the efficiency of patient care.
- At this pivotal moment, the implementation of ISO 80369 is crucial in preventing misconnections of small-bore connectors utilized in healthcare for liquids and gases. This standard is designed to enhance patient safety by guaranteeing appropriate device connections, especially in critical areas such as enteral feeding, respiratory systems, and intravenous infusions. The standard is divided into multiple sections, each focusing on particular applications and types of connectors.
- ISO 80369-1:2018 Small-bore connectors for liquids and gases in healthcare applications Part 1: General requirements
- ISO 80369-2:2024 Small-bore connectors for liquids and gases in healthcare applications Part 2: Connectors for respiratory applications
- ISO 80369-3:2016/Amd 1:2019 Small-bore connectors for liquids and gases in healthcare applications Part 3: Connectors for enteral applications
- IEC 80369-5:2016 Small-bore connectors for liquids and gases in healthcare applications Part 5: Connectors for limb cuff inflation applications
- ISO 80369-6:2016 Small bore connectors for liquids and gases in healthcare applications Part 6: Connectors for neuraxial applications
- ISO 80369-7:2021 Small-bore connectors for liquids and gases in healthcare applications Part 7: Connectors for intravascular or hypodermic applications
- ISO 80369-20:2024 Small-bore connectors for liquids and gases in healthcare applications Part 20: Common test methods
ISO 80369 aims to prevent misconnections between medical devices by using unique connector designs for different applications. These designs are based on human factors engineering and computer-aided design (CAD) analysis to ensure connectors only connect to their intended mating connectors. The goal is to make it physically difficult, if not impossible, to connect unrelated systems.
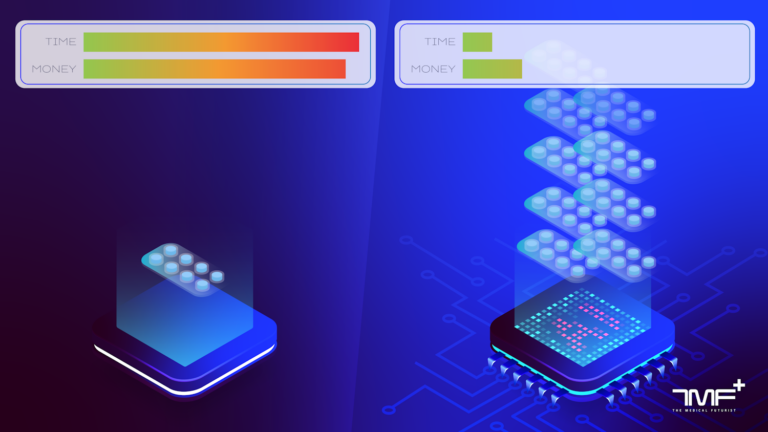
Adhering to the 80369 standard and ensuring compliance provides advantages for medical device manufacturers, healthcare personnel, and, most crucially, patients. Conforming to this harmonized standard enhances patient safety and alleviates the workload of hospital staff. The time saved through improved design, as opposed to relying on manual controls to prevent misconnections, can be effectively redirected towards enhancing patient care.
References:
The post Significance of Harmonized standards appeared first on MedTech Intelligence.